Lockdowns don’t work.
That simple sentence is enough to ignite a firestorm of controversy these days, whether you say it in public (to someone at least six feet away, of course) or online. As soon as the words leave your lips, they begin to be interpreted in extraordinary ways. Why do you want to kill old people? Why do you think the economy is more important than saving lives? Why do you hate science? Are you a shill for Trump? Why are you spreading misinformation about the severity of COVID?
But here’s the thing: there’s no evidence of lockdowns working. If strict lockdowns actually saved lives, I would be all for them, even if they had large economic costs. But, put simply, the scientific and medical case for strict lockdowns is paper-thin.
Here’s the thing: there’s no evidence of lockdowns working. If strict lockdowns actually saved lives, I would be all for them, even if they had large economic costs. But the scientific and medical case for strict lockdowns is paper-thin.
Start your day with Public Discourse
Sign up and get our daily essays sent straight to your inbox.What Works and What Doesn’t
Before I can explain exactly why lockdowns don’t work, we need to define what “lockdowns” are and, especially, what they are not. I define lockdowns as having three characteristics. First, people are ordered to stay at home or required to provide a reason for movement outside of home. Second, assemblies are limited to a very small (usually single-digit) threshold. Third, many businesses and activities are forced to close, even if they do not technically constitute assemblies and would like to stay open. Stay-at-home orders, low assembly thresholds, and business closures together constitute a lockdown. Without those three features, it’s not a lockdown.
School cancellations aren’t lockdowns. Not only do school cancellations have excellent scientific research to support their use as epidemic-fighting tools, but I simply don’t accept the idea that we are harming children or families by forcing kids to be at home with their parents more and learn online or, God forbid, read books.
[Read: Leisure In a Time of Coronavirus]
Travel restrictions, like setting up interstate checkpoints with mandatory testing at state borders, are not lockdowns. They are another time-tested strategy for disease-fighting. Travel restrictions are highly effective and, while a great inconvenience, aren’t actually forcing you to stay “locked down” at home.
Moderate assembly limits, such as bans on assemblies over 100 people, are not lockdowns. Most major COVID outbreaks have been linked to large gatherings of people, so such bans make scientific sense, even as they also represent fairly modest restrictions on individual behavior.
Centralized quarantine orders, where individuals who test positive or individuals who have had contact with COVID-infected people are forced to be quarantined for seven, fourteen, or twenty-one days in hotels or special-purpose spaces are an extremely effective way to fight disease. In fact, this is how Moses, in Leviticus, commands the Israelites to combat infectious disease, and it’s the strategy used to keep COVID at bay here in Hong Kong, where I live, too. Centralized quarantines dramatically restrict the liberties of a small share of the population in order to afford some degree of normalcy to the vast majority.
[Read: Pandemics and the Agency of Citizens]
Requirements that people wear masks are not lockdowns; they are good sense. Respiratory diseases are spread through respiratory droplets. Masks are scientifically proven to reduce how many such droplets are spread by infected people. Because many infected people are asymptomatic, it’s important that everyone wear a mask. Jogging down the sidewalk? Wear a mask! At a restaurant? Wear a mask! Sitting at your desk at work? Wear a mask! Universal mask-wearing is one of the single best ways to reduce the spread of respiratory diseases.
Lockdowns don’t work. These other policies—travel restrictions, large-assembly limits, centralized quarantine, mask requirements, and school cancellations—do work. Because COVID is an extremely severe disease that, if left unchecked, will kill hundreds of thousands of Americans, it is vitally important that policymakers focus their efforts on policies that do work (masks, central quarantines, travel restrictions, school cancellations, large-assembly limits), and avoid implementing draconian, unpopular policies that don’t work (lockdowns).
The Best Evidence for Lockdowns
At this point, the question I usually get is, “What’s your evidence that lockdowns don’t work?”
It’s a strange question. Why should I have to prove that lockdowns don’t work? The burden of proof is to show that they do work! If you’re going to essentially cancel the civil liberties of the entire population for a few weeks, you should probably have evidence that the strategy will work. And there, lockdown advocates fail miserably, because they simply don’t have evidence.
If you’re going to essentially cancel the civil liberties of the entire population for a few weeks, you should probably have evidence that the strategy will work.
There are very few documented cases of lockdowns being used to fight epidemic diseases in the past. One example where lockdowns were used was to fight Ebola in West Africa. However, it’s hard to study these lockdowns, since they also included a door-to-door campaign delivering information and supplies to almost 70 percent of the impacted areas. Untangling the effect of lockdowns and the effect of information is difficult. It’s so difficult that this article will focus exclusively on lockdowns, and I will have a follow-up post discussing the role of information.
Nor does the 1918 influenza pandemic provide much help to lockdown advocates. The most severe restrictions during that pandemic, which dramatically reduced deaths, were in St. Louis. St. Louis’s measures included closures of specific assemblies like churches, closure of all “amusements,” restricted business hours, mask orders, school cancellations, and centralized quarantine procedures. St. Louis never issued a stay-at-home order, and only imposed a complete cancellation of business for about forty-eight hours.
Thus, lacking many prior cases to study, any evidence in support of lockdowns must come from the fight against COVID-19 itself.
The best evidence comes from Wuhan, where China imposed a strict lockdown in late January. Researchers have found that this lockdown, combined with other prior policies, as well as population behavioral changes, may have reduced the reproduction rate of the disease from 3.9 to 1.3: a big change, but not enough to prevent the spread of the disease. In Wuhan, the reproductive rate did not drop to 0.3, a level at which the disease can truly be beaten, until after centralized quarantine measures had been put in place. It was centralized quarantine that beat COVID in Wuhan, not lockdowns.
The Cases of Spain and Italy
But while the data from Wuhan support my argument that lockdown effects are far more modest than advocates claim, it’s not clear if Chinese data should be trusted. For better examples, we need to turn to countries with reliable data. We can also look at countries that implemented lockdowns, and what has happened to their death tolls since.
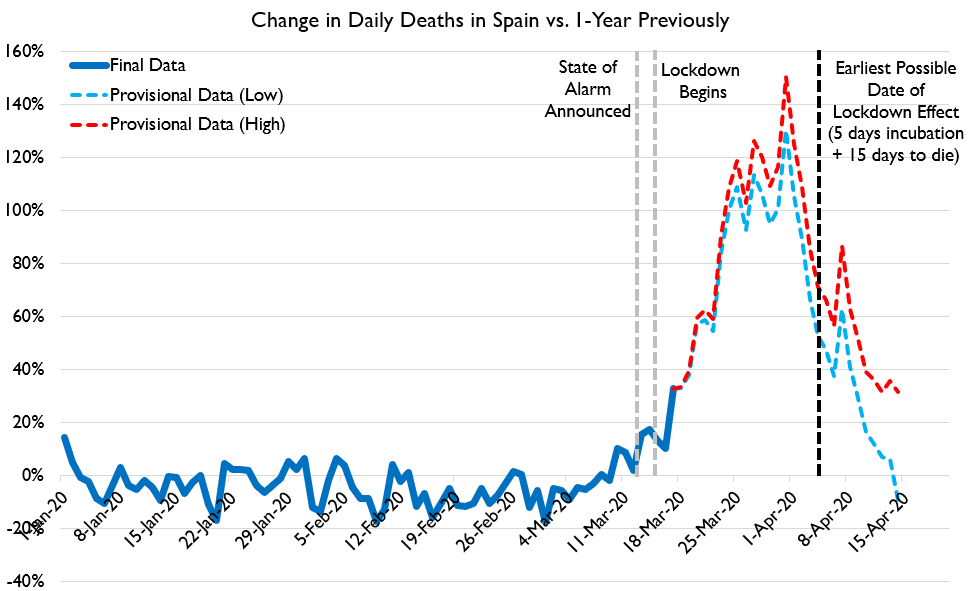
Figure 1 below shows the change in daily deaths from all causes in Spain on a given date in 2020 versus 365 days earlier. Looking at all causes of death neatly sidesteps thorny issues around defining COVID deaths, and captures a credible, reliable metric that nobody seriously disputes.
At this point, enough research has been done that it’s possible to say with some confidence about how long it takes to die of COVID. Across numerous medical studies, COVID has reliably been found to take anywhere from two to ten days to incubate (but most usually four to six days), and from twelve to twenty-four days to kill a person after incubation. Across all studies, these estimate places typical death time at about twenty to twenty-five days after first exposure.
The only exception to this finding of “approximately twenty days to die from exposure” is a data brief from Italy, which found time from symptom onset to death of a mere ten days. However, it’s not clear how rigorously the data on symptom onset were being tracked, as the data brief provides no methodology or details about the estimate. It’s possible the symptoms being defined as onset represent a later progression of the disease than the symptoms tracked in other studies. And even then, for those patients transferred to ICU (that is, those experiencing severe respiratory symptoms driving the typical death from COVID), time from onset to death was nearer eighteen days, which, plus a few days for disease incubation, puts time to death at or above twenty days from first exposure.
As such, practically speaking, lockdowns should not create an appreciable decline in deaths earlier than twenty days after a lockdown. If deaths begin to decline very rapidly after a policy measure is put in place, it suggests the real force reducing deaths occurred much earlier.
What we see in Spain’s case, however, is that the spike in deaths plateaued around March 25–30, just ten to fifteen days after the lockdown, and began to fall about eighteen days after the lockdown. Put plainly, it appears to be the case that COVID infections were already declining before Spain went into lockdown. Dramatic declines began two to five days before lockdown. Notably, COVID began to be a huge news item in Spain around March 5–10, as regional governments noticed community spread and began closing down large events (for example, Catalonia restricted events over 1,000 people on March 9, and on March 12 schools began to be shut down). But perhaps most notably of all, on March 13, Spain declared a “State of Alarm,” which put the whole country on alert. School cancellations. Large assembly bans. Extensive public notice. These kinds of measures are all a much tighter fit to Spain’s mortality patterns.
The Cases of France and Lombardy
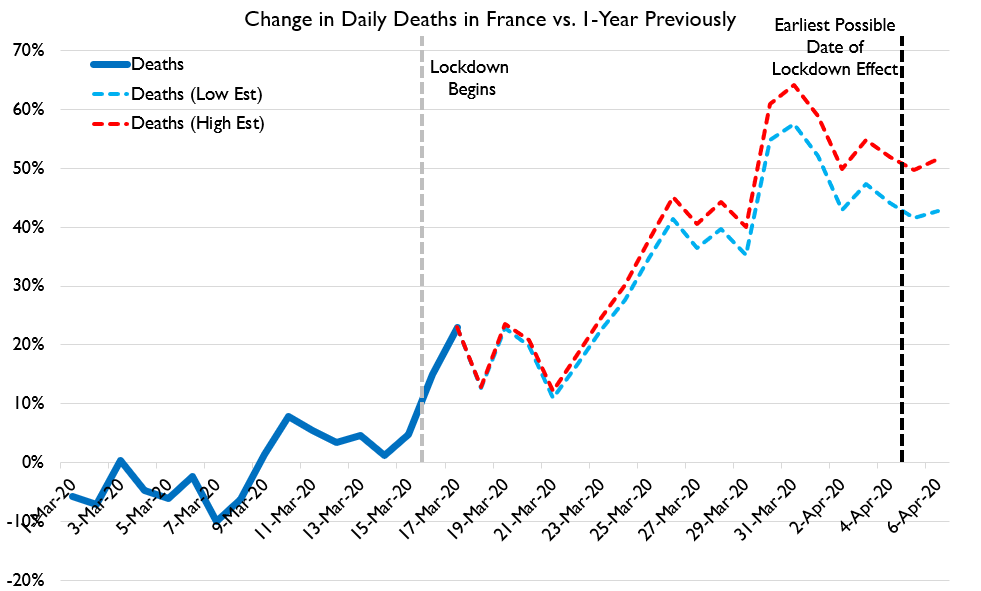
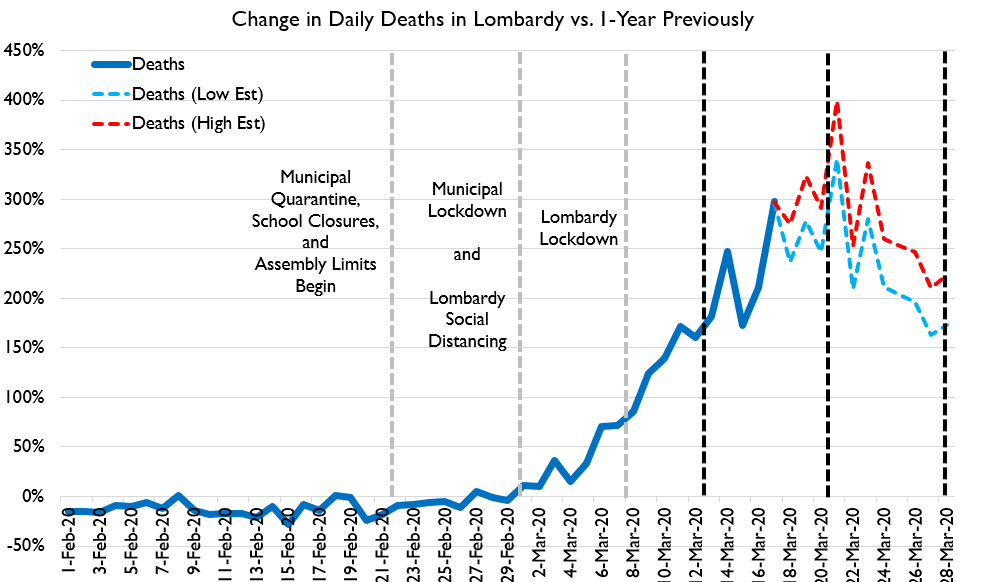
We can also look at France. France’s data are not quite as recently updated as Spain’s, and thus less can be concluded from them. France went into lockdown on March 16, but the spike in deaths appears to have more or less stabilized some time between March 25 and April 6—thus, again, before the lockdown could have saved lives by preventing infections.
Figure 3 looks at the experience of the Lombardy region of Italy, marking each major phase of control measures, and when they might have had an effect on deaths. Again, the death spike in Lombardy had already plateaued or even begun to decline before the region-wide lockdown could have been responsible. Indeed, it appears that the very modest municipal lockdowns of March 1 in extremely hard-hit areas, along with region-wide cancellation of school and large assemblies, may have been the actual trigger for declining deaths. The timing of death declines simply does not match the timing of lockdowns.
The same lack of correlation shows up in virtually all eleven cases I could find with publicly available data on total deaths in areas that have had COVID lockdowns. Across those eleven areas, the average region saw its death spike begin to decline about fifteen days after it went into lockdown, five days too early for even the most optimistic theories on what a lockdown might do.
Successful Control without Lockdown
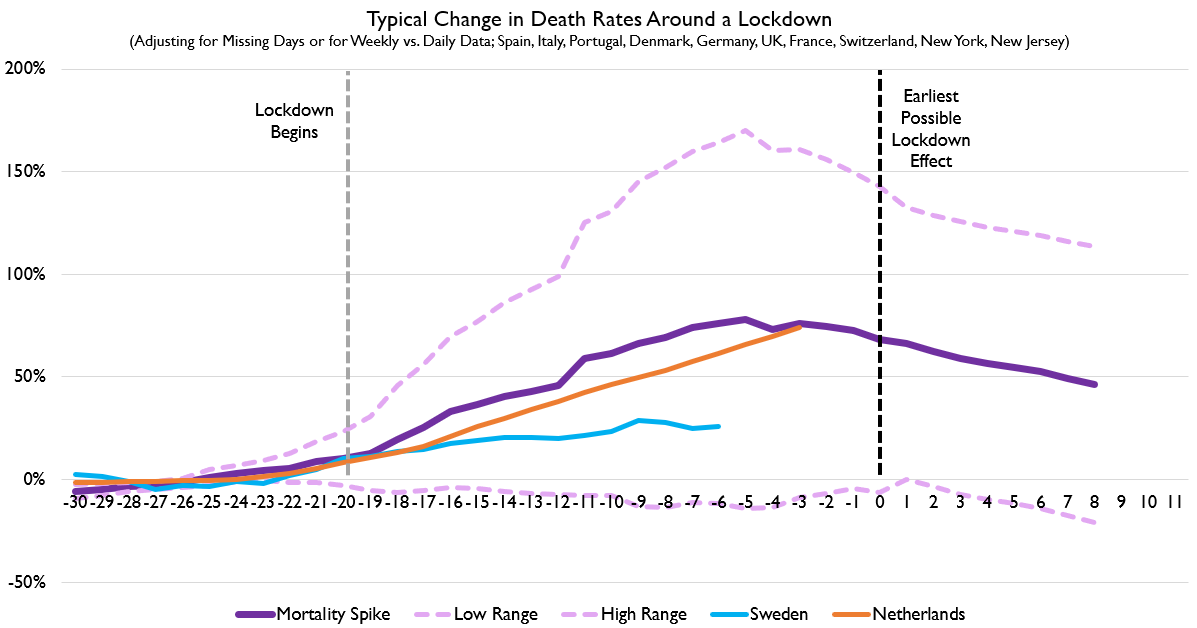
But we can also compare countries that went into lockdown to two major regions that did not go into lockdown: Sweden and the Netherlands. Doing so is a bit tricky: we can easily align lockdown countries together based on the date of their lockdowns. But where should Sweden and the Netherlands fall in that realignment of time series, given that they have not had a lockdown? My method is simple: in the average region with a lockdown, the lockdown was imposed when deaths were running about 10 percent higher than a year earlier. So I shift the data for Sweden and the Netherlands so that their day when deaths were first 10 percent above a year earlier are aligned with the day when other countries imposed lockdowns. This is a way of saying, “What might Sweden or the Netherlands have looked like if they imposed a lockdown at the same point in their outbreak as other lockdown countries did?”
Sweden is performing much better than the typical locked-down country. The Netherlands is having similar performance. This is all consistent with the idea that lockdowns are not a decisive factor in determining the scale of mortality a society experiences during an outbreak of COVID-19.
Aside from mortality data, it’s worth taking a look at the countries that have had the most successful control efforts, like Hong Kong, Taiwan, and Korea. None of these countries ever went into lockdown. In Hong Kong, where I live, we received a very large number of imported cases in recent weeks, but they did not lead to a large outbreak. We still have had just four deaths and only about a thousand cases, in a region of 7.5 million people. Recent data suggest that the reproductive rate of COVID-19 in Hong Kong is around 0.3, the same level that was measured in Wuhan after it imposed lockdowns and centralized quarantine. Notably, Hong Kong has not had a lockdown, but it does have a program of centralized quarantine: those who test positive for COVID, as well as anyone they have had contact with, are quarantined in a designated site like a hotel or a government facility.
The Data from the United States
But we don’t have to look beyond the United States for evidence of whether lockdowns work: we can simply compare how different US counties have performed over time.
[Read: The Strange Battle of Staying Home]
I’ve built a model to predict county-level deaths per 100,000 people as of April 19. My specific interest is to know if policies like stay-at-home orders reduce deaths. Luckily, the research team at Johns Hopkins University has coded up what measures are in place for every county, and when they were put in place. I have merged this with county-level data like density, metro area size, college-educated share, racial mix, population share born in Italy (a good measure of exposure to European outbreaks), transit-usage, and how long it has been since a county’s first death (a good measure of duration of exposure to a COVID outbreak), to produce a statistical regression with a similar structure as that used by other researchers.
My findings are striking: for every eight days (including weekends) since school cancellations began, a county tends to have one less death per 100,000 people. For every nine days a ban on gatherings over 500 people has been in place, there’s one less death per 100,000 people. These policies work. But the correlation flips for bans on gatherings of fifty people or for stay-at-home orders. For every two weeks a stay-at-home order is in place, the death rate rises by one person per 100,000. For bans of gatherings of fifty people, it’s every eleven days.
Because I controlled for how long it’s been since the first county death, this is probably not being driven by harder-hit places choosing to adopt tougher policies. But just to check, I also added a control for the deaths per 100,000 people in each county on March 31. This does reduce the size and significance of effects for each policy, but not the relationship between them. Nor are my findings changed by excluding the New York City metro area, or adding or removing a handful of other variables related to climate, industry or occupation mix, rurality, etc. All the underlying data can be downloaded publicly.
The only US-based academic study empirically linking lockdowns to lower deaths is a recent economics paper identifying California’s lockdown as the reason for its lower death rate. The problem with this paper is that the authors find that the lockdown began to reduce California’s deaths just five days after being implemented. The effect is too early to derive from the supposed cause. My goal is not to prove that stay-at-home orders increase COVID deaths; that’s a strong claim I wouldn’t venture. My goal is simply to show that there is not currently any evidence that lockdowns work. None of the actual examples of lockdowns around the world provides particularly compelling evidence that lockdowns actually work.
Adopt What Works, Not What Doesn’t
We don’t need to have a national debate about whether the economic costs of lockdowns outweigh their public health benefits, because lockdowns do not provide public health benefits.
We don’t need to have a national debate about whether the economic costs of lockdowns outweigh their public health benefits, because lockdowns do not provide public health benefits.
Many policies do provide public-health benefits. Masks work and should be mandatory, just as they were during the 1918 influenza pandemic. School cancellations are hugely important, and reliably show up as a key part of reducing infection. Bans on large assemblies are an obvious policy with good support. Restrictions on long-distance travel help reduce the occurrence of new outbreaks. Centralized quarantine helps actively reduce the spread of COVID-19 to a very low level.
But ordering people to cower in their homes, harassing people for having playdates in the park, and ordering small businesses to close up shop regardless of their hygienic procedures simply has no demonstrated effectiveness. These policies should be replaced by stringent mask requirements, large-scale centralized quarantine protocols, and renewed emphasis on empowering people to protect themselves and their neighbors by adopting social distancing during their everyday life.